SGLT2i / GLP-1 Combo: More Kidney Protection?
SGLT2i / GLP-1 Combo: Chronic kidney disease (CKD) is a common and serious complication of type 2 diabetes mellitus (T2DM). The kidney damage in diabetes is multifactorial: hyperglycemia, hypertension, glomerular hyperfiltration, oxidative stress, inflammation, lipid abnormalities, and others all contribute to progressive loss of nephron function. Preventing or slowing progression to end-stage kidney disease (ESKD) is a key goal in managing patients with T2DM.
Over the last decade, two classes of antidiabetic agents have emerged not just for glycemic control, but also for their cardiorenal protective effects: the sodium–glucose co-transporter 2 inhibitors (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP-1RAs). Each has been shown in large randomized controlled trials (RCTs) and real-world studies to reduce risks of kidney disease progression, albuminuria, heart failure, and cardiovascular mortality. The question arises: when used in combination, do SGLT2 inhibitors and GLP-1 receptor agonists provide additive or synergistic kidney protection beyond what either class offers alone?
This article explores that question—examining the biological mechanisms, clinical evidence, advantages, limitations, and future directions of SGLT2i and GLP-1RA combination therapy.
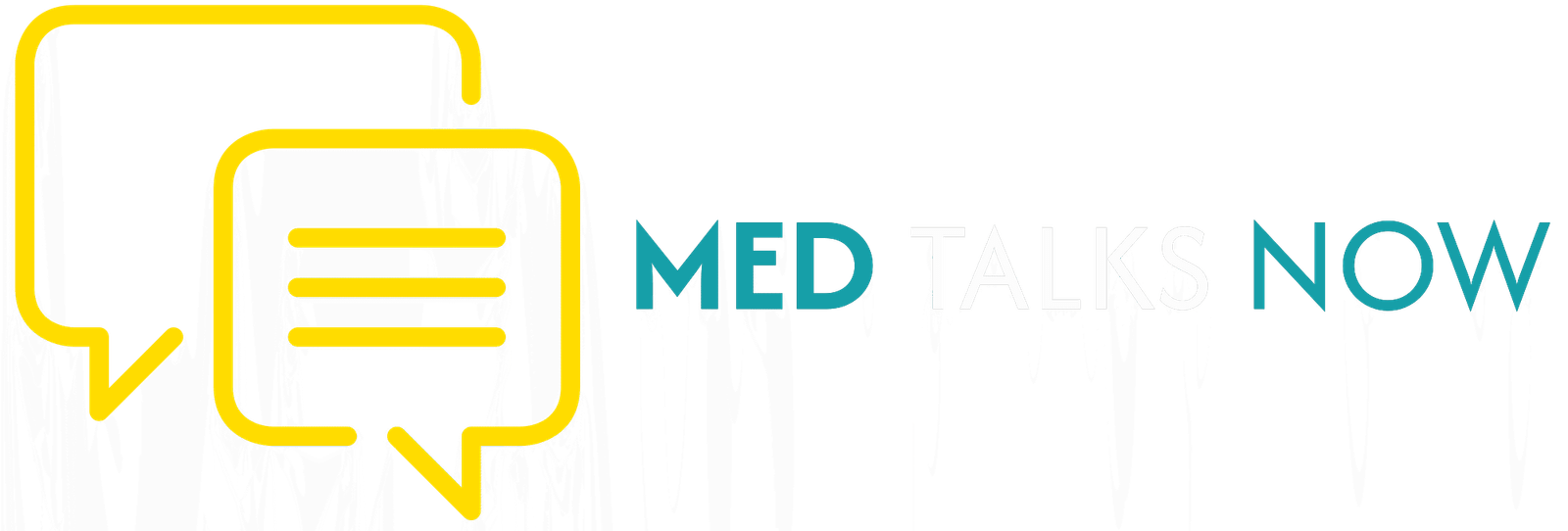
Mechanisms of Renoprotection: How SGLT2i and GLP-1RA Work (Separately and Together)
To understand the potential of the combination, it is necessary to review how each class impacts kidney pathology and how their mechanisms might complement each other.
SGLT2 inhibitors
SGLT2, located in the proximal tubule of the nephron, reabsorbs filtered glucose. Inhibition leads to:
- Glycosuria: lowering blood glucose levels.
- Osmotic diuresis and natriuresis: increasing sodium excretion, reducing intravascular volume and glomerular hyperfiltration.
- Reduction in intra-glomerular pressure: through restoration of tubuloglomerular feedback.
- Lower blood pressure and weight loss via diuresis and caloric loss.
- Metabolic effects: improved mitochondrial function and energy efficiency.
- Non-glycemic effects: reduced inflammation, oxidative stress, and fibrosis.
Clinical trials such as CREDENCE, DAPA-CKD, and EMPA-Kidney have shown that SGLT2 inhibitors slow eGFR decline, reduce ESKD, and lower albuminuria, establishing them as cornerstone agents for renal protection.
GLP-1 receptor agonists
GLP-1RAs mimic the incretin hormone GLP-1, which enhances insulin secretion, suppresses glucagon, slows gastric emptying, and reduces appetite. Beyond glucose control, they have additional benefits:
- Weight reduction and improved metabolic profile.
- Blood pressure lowering through vasodilation and natriuresis.
- Anti-inflammatory and antioxidant effects, reducing endothelial and glomerular injury.
- Reduction in albuminuria and improved composite kidney outcomes in trials such as LEADER, SUSTAIN-6, and REWIND.
While the renal benefits of GLP-1RAs have mostly been secondary outcomes, the consistent trends indicate meaningful kidney protection.
Why Combined Therapy May Be Better
The rationale for combining SGLT2i and GLP-1RA is based on their complementary mechanisms:
- SGLT2i targets hemodynamic and tubular pathways; GLP-1RA acts on metabolic, vascular, and inflammatory pathways.
- Together, they address multiple contributors to diabetic kidney disease—hyperglycemia, obesity, hypertension, inflammation, and oxidative stress.
- Both promote weight loss and blood pressure reduction, amplifying kidney protection.
- GLP-1RA may counteract medullary hypoxia associated with SGLT2 inhibition, offering physiological balance.
The biological plausibility is strong, suggesting that combined use could provide more comprehensive renoprotection.
Clinical and Real-World Evidence for Kidney Outcomes with the Combination
Post Hoc Analyses
In the RECAP study involving 643 T2DM patients, those who started an SGLT2 inhibitor first and later added a GLP-1RA experienced a significant slowing of annual eGFR decline—from approximately −3.5 to −0.4 mL/min/1.73m² per year. Patients who started with GLP-1RA and later added SGLT2i also showed improvement, though less pronounced.
Another analysis using global health network data reported that combination therapy reduced the risk of major adverse kidney events (MAKE)—including acute kidney injury (AKI), ESKD, and all-cause mortality—compared with SGLT2i monotherapy.
Real-World Cohort Studies
Large observational studies confirm these findings. In a U.S. cohort of over 100,000 patients, those on the SGLT2i + GLP-1RA combination showed better kidney function trajectories, lower cardiovascular events, and improved metabolic outcomes compared to those on SGLT2i alone.
A separate population-based study comparing SGLT2i and GLP-1RA monotherapies found SGLT2i users had lower risk of ESKD and slower eGFR decline, reinforcing the renal potency of the class. When used together, the benefits appeared additive.
Meta-Analyses and Consensus Recommendations
Meta-analyses indicate that adding SGLT2 inhibitors to GLP-1RA therapy can reduce the risk of kidney disease progression by roughly one-third and slow annual kidney function loss by nearly 60% compared with GLP-1RA alone.
International expert groups, such as EURECA-m and DIABESITY, now highlight the potential of this combination for enhanced cardiorenal protection in T2DM with CKD.
Kidney Outcomes Observed
Across studies, key renal benefits observed include:
- Slower eGFR decline over time.
- Reduced progression to ESKD or sustained doubling of serum creatinine.
- Lower incidence or worsening of albuminuria.
- Decreased risk of acute kidney injury and composite renal events.
Advantages of Combination Therapy
- Comprehensive Pathway Coverage
The combination addresses multiple mechanisms—hemodynamic stress, metabolic imbalance, inflammation, and oxidative damage—providing multi-targeted kidney protection. - Additive Metabolic Benefits
GLP-1RA contributes substantial weight loss and glycemic improvement, complementing SGLT2i’s effects on blood pressure and volume regulation. - Cardiovascular Protection
Since cardiovascular and renal diseases share common mechanisms, the combination also delivers enhanced heart protection, reducing the risk of heart failure and atherosclerotic events. - Potential Delay in Disease Progression
Greater protection may delay CKD progression, reducing the need for dialysis or transplantation. - Improved Suitability Across CKD Stages
Evidence supports benefit in both early and moderate CKD, making it adaptable to a wide patient population.
Limitations, Risks, and Uncertainties
- Lack of Dedicated RCTs
Most data come from post hoc analyses or real-world studies rather than large RCTs designed specifically for kidney outcomes with combination therapy. - Cost and Accessibility
GLP-1RAs, especially injectable ones, can be expensive, limiting access in some regions. Combination therapy increases cost and complexity. - Side Effects
- GLP-1RAs may cause nausea, vomiting, and gastrointestinal discomfort.SGLT2 inhibitors may lead to genital infections, dehydration, or euglycemic ketoacidosis in susceptible individuals.
- Combining them may increase the risk of cumulative side effects.
- Efficacy in Advanced CKD
SGLT2i effectiveness diminishes as eGFR drops below 30 mL/min/1.73 m². Data for combination use in advanced CKD remain limited. - Population Heterogeneity
Benefits may vary depending on age, baseline renal function, albuminuria, and comorbidities such as heart failure or obesity. - Long-Term Safety Data
While short- to mid-term outcomes are encouraging, long-term effects beyond five years are still under investigation.
Where Evidence Is Strongest and What We Still Don’t Know
Strong Evidence
- Combination therapy slows eGFR decline and reduces albuminuria progression.
- Observational data consistently show fewer renal events compared with monotherapy.
- Meta-analyses and consensus guidelines endorse combination therapy for high-risk diabetic patients.
Knowledge Gaps
- Need for head-to-head RCTs evaluating renal endpoints directly.
- Identification of subgroups deriving maximum benefit.
- Determining optimal initiation timing in the course of CKD.
- Clarifying long-term cost-effectiveness and safety profiles.
Practical Considerations for Clinicians
1. Baseline Assessment
Evaluate eGFR, albuminuria, cardiovascular status, and risk factors for volume depletion or gastrointestinal intolerance before initiating therapy.
2. Choice of Agents
Different drugs within each class have distinct renal data and tolerability. Agents like empagliflozin or dapagliflozin (SGLT2i) and semaglutide or liraglutide (GLP-1RA) have the most robust renal and cardiovascular evidence.
3. Monitoring
- Check kidney function periodically.
- Watch for initial eGFR “dip” with SGLT2i, which usually stabilizes.
- Monitor hydration status, electrolytes, and gastrointestinal tolerance.
4. Patient Education
Explain potential side effects, importance of hydration, hygiene to prevent infections, and adherence to therapy.
5. Integration with Other Therapies
Combination therapy should complement, not replace, lifestyle interventions, blood pressure control, and statin use.
Key Studies at a Glance
| Study / Analysis | Population | Key Finding |
| RECAP (post hoc) | 643 T2DM patients | Slower eGFR decline when SGLT2i was initiated before GLP-1RA. |
| TriNetX Global Network | Large real-world database | Combo therapy lowered risk of acute kidney injury, ESKD, and death vs SGLT2i alone. |
| U.S. Retrospective Cohort (100,000+) | T2DM with and without CKD | Improved kidney function and cardiovascular outcomes with combo therapy. |
| Comparative Monotherapy Study | Population-based T2DM cohort | SGLT2i superior to GLP-1RA in renal preservation; combination likely additive. |
Potential Risks and Side Effects
- Gastrointestinal discomfort from GLP-1RAs.
- Volume depletion and hypotension with SGLT2i.
- Genital or urinary tract infections due to glycosuria.
- Hypoglycemia risk is low unless used with insulin or sulfonylureas.
- Euglycemic ketoacidosis is rare but possible in dehydrated or fasting patients.
- Cost burden remains a major limiting factor in widespread use.
Implications for Guidelines and Clinical Practice
Recent diabetes and kidney disease guidelines increasingly emphasize early introduction of both SGLT2 inhibitors and GLP-1 receptor agonists for patients with T2DM and high cardiovascular or renal risk.
The treatment paradigm is shifting from a glucose-centric to an organ-protective approach. Instead of waiting for poor glycemic control, clinicians are encouraged to start these agents early to preserve kidney and cardiovascular health.
This shift requires coordinated patient education, cost considerations, and system-level support to ensure accessibility.
Future Research Directions
- Dedicated RCTs comparing combination vs monotherapy on primary renal outcomes.
- Stage-specific analysis to identify when in CKD progression combination therapy is most effective.
- Comparative studies of specific drug pairings and new dual-agonists (GLP-1/GIP).
- Long-term safety monitoring beyond five years.
- Cost-effectiveness assessments in different healthcare settings.
- Mechanistic studies using biomarkers and imaging to explore renal oxygenation and fibrosis modulation.
Conclusion
The combination of SGLT2 inhibitors and GLP-1 receptor agonists represents a promising frontier in diabetic kidney disease management. Each class individually improves kidney and cardiovascular outcomes through distinct yet complementary pathways. When used together, they appear to offer additive—or possibly synergistic—protection against kidney function decline.
Real-world and post hoc analyses show slower eGFR loss, reduced albuminuria, and fewer adverse kidney events with combination therapy compared to either agent alone. Although the absence of dedicated large-scale RCTs leaves some uncertainty, current evidence supports their concurrent use in appropriate patients, particularly those with type 2 diabetes and elevated renal or cardiovascular risk.
Clinicians should evaluate patient suitability carefully, considering renal function, comorbidities, tolerability, and cost. As the evidence base grows, SGLT2i + GLP-1RA therapy is likely to become a central strategy in comprehensive kidney and cardiovascular protection for people with diabetes.
Read Also- Asthma Inhalers & Climate Change: A Hidden Environmental Impact
Tags- SGLT2 inhibitors, GLP-1 receptor agonists, kidney health, diabetic nephropathy, type 2 diabetes, renal protection, cardiovascular health, combination therapy, diabetes treatment, kidney disease prevention